Bioimpacts. 12(5):439-448. doi: 10.34172/bi.2022.22132Original Research
Reduced inflammation following human endometrial stromal/stem cell injection into male Wistar rats with cisplatin-induced acute kidney injury
Hadis Zeinali 1 , Mahnaz Azarnia 1, *
, Mahnaz Azarnia 1, * , Peyman Keyhanvar 2, 3, *
, Peyman Keyhanvar 2, 3, * , Reza Moghadasali 4, Somayeh Ebrahimi-Barough 5, Majid Marandi-Kouchaki 1
, Reza Moghadasali 4, Somayeh Ebrahimi-Barough 5, Majid Marandi-Kouchaki 1
1Department of Animal Biology, Faculty of Biological Sciences, Kharazmi University, Tehran, Iran
2Stem Cell Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Medical Nanotechnology, School of Advanced Medical Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
4Department of Stem Cells and Developmental Biology, Cell Sciences Research Center, Royan Institute for Stem Cell Biology and Technology, ACECR, Tehran, Iran
5Department of Tissue Engineering and Applied Cell Sciences, School of Advanced Technologies in Medicine, Tehran University of Medical Sciences, Tehran, Iran
*Corresponding authors: Mahnaz Azarnia, Email: azarnia@khu.ac.ir; Peyman Keyhanvar, Email: regenerative.md@gmail.com
Abstract
Introduction:
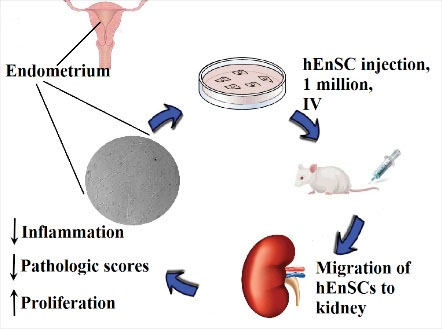
Inflammation is one of the most important mechanisms involved in cisplatin-induced acute kidney injury (AKI). Mesenchymal stromal/stem cells (MSCs) exhibit anti-inflammatory and immunomodulatory abilities. Human endometrial stromal/stem cells (hEnSCs) exhibit similar properties to MSCs. These cells secrete immunoregulators, so we investigated the inflammatory aspect of hEnSCs in the treatment of cisplatin-induced AKI in Wistar rats.
Methods:
Each group consisted of 6 male Wistar rats. Groups were as follows: sham, model (5 mg/kg cisplatin, IP), and treatment (1 million hEnSCs, IV, 3 hours after cisplatin). Renal function, histopathology, proliferation rate, infiltration of CD3+ T cell, and expression of Il-10 and cystatin c (Cst3) were assessed on day 5. DiI-labeled cells were tracked in kidney and liver on days 4 and 14.
Results:
HEnSC transplantation improved cisplatin-induced injuries such as renal dysfunction and tissue damage. The highest levels of pathologic scores and hyaline cast formation were observed in the model group while hEnSCs transplantation resulted in their reduction (154.00 ± 14.95, 8.00 ± 1.41 vs. 119.40 ± 5.43, 2.50 ± 1.05). The percentage of Ki-67 positive cells in the treatment group increased while cisplatin decreased proliferation (39.91 ± 5.33 vs. 23.91 ± 3.57 in glomeruli and 39.07 ± 2.95 vs. 16.61 ± 3.25 in tubules). The expression of Cst3 and Il-10 was higher in the model and treatment groups, respectively. DiI-labeled cells were observed in the renal tubules and liver lobes on days 4 and 14.
Conclusion:
HEnSCs may ameliorate cisplatin-induced AKI through anti-inflammatory and immunomodulatory effects and/or through paracrine effects.
Keywords: Inflammation, Human endometrial stromal/stem cell, Rat, Cisplatin, Acute kidney injury
Copyright
© 2022 The Author(s).
This work is published by BioImpacts as an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Introduction
Acute kidney injury (AKI) is a public health problem due to high costs, mortality even in young adults especially in developing countries, increased risk of chronic kidney disease (CKD) and end-stage renal disease (ESRD), and decreased quality of life among the survivors. About 13.3 million people are affected by AKI annually. AKI is defined as a rapid decline in renal function due to various insults.
1
Cisplatin or cis-diamminedichloroplatinum (II) is a powerful choice in the first-line treatment of solid cancers, though it has side effects such as nephrotoxicity. AKI occurs in about 30% of patients receiving cisplatin alone or in combination. The pathology of cisplatin-induced AKI includes tubular and vascular damage, oxidative stress, cell death, and inflammation following the entry of cisplatin into cells.
2
Appropriate treatment should be able to reduce morbidity and mortality and improve kidney function. Pharmaceutical agents only relieve AKI symptoms without renal regeneration.
3
Resistant inflammation is the main cause of renal diseases, which is drug resistant. Dialysis is time consuming and expensive and is not a complete replacement for the kidney. Anemia, pericarditis or inflammation of pericardium, infection of the bloodstream, sudden cardiac death, and so on are among the risks of dialysis.
4
Kidney transplantation is an expensive therapy that increases the risk of cardiovascular disease, cancer, graft versus host reaction, and infection.
5
Stem cell-based therapy replaces or repairs injured cells, tissues, and organs. This treatment can result in considerable changes in the treatment of human disease and functional recovery of the affected parts.
6
Stem cell-based therapies will play a great role in the future of regenerative medicine.
Using cells extracted from living organisms in treatment is a brilliant procedure to maintain the quality of regenerative medicine.
7
Mesenchymal stromal/stem cells (MSCs) are an amazing type of stem cells that are present in almost all human tissues. MSCs secrete variety of growth factors and cytokines; therefore, these cells play a role in tissue repair. MSCs are known for their anti-apoptotic, anti-fibrotic, antioxidative, anti-inflammatory, proangiogenic, and immunomodulatory properties. Therefore, MSC based- cell therapy is a clever choice for AKI because of its unique properties.
8
Bone marrow-derived stem cells (BM-MSCs) are more suitable for regenerating solid tissues.
9
Human endometrial stromal/stem cells (hEnSCs), which separate from uterine endometrium, exhibit similar properties to MSCs. HEnSCs express MSC surface antigens for example CD73, CD90, and CD105, while lacking hematopoietic and endothelial surface markers. These cells secrete immune regulators such as IDO, PGE2, and IL-6 that suppress T and natural killer (NK) cells. IDO, PGE2, and IL-6 can reprogram monocytes and macrophages into M2 or an anti-inflammatory phenotype with high IL-10 secretion. PGE2 also promotes epithelial cell proliferation. The mentioned properties have suggested hEnSCs as a novel cell therapy for disorders of endometrium through the immunomodulation and tissue repair.
10
Inflammatory responses are one of the most important mechanisms involved in AKI pathology due to cisplatin. Immune cells such as macrophages and T cells infiltrate the kidney during injuries caused by cisplatin and ischemia.
11,12
On the other hand, as mentioned, hEnSCs have anti-inflammatory properties. The effect of hEnSCs on AKI in terms of reducing inflammation has not been studied. Hence we investigated the inflammatory aspect of hEnSCs in the treatment of cisplatin-induced AKI.
Materials and Methods
Preparation of hEnSCs, adipogenic, and osteogenic differentiations
Briefly, we obtained the written consent of the donor. HEnSCs were isolated from human endometrial biopsy using collagenase type I. Flow cytometry was performed on P3 cells.
13
Cells were cultured in DMEM with 10% FBS and maintained in a CO2 incubator (5% CO2, 37°C). To induce adipogenic differentiation in the third passage, we platted 1×104 cells in a 35-mm culture dish, which was incubated for 48 hours after reaching the confluence. The differentiation medium included: DMEM/F12, 10% FBS, 1% penicillin-streptomycin (pen/strep) or 100 IU/mL penicillin and 100 μg/mL streptomycin, 10 µM insulin, 60 µM indomethacin, 1 µM dexamethasone (all from Sigma-Aldrich, USA). The incubation period lasted 28 days and the differentiation medium was changed every 3-4 days. We also investigated osteogenic differentiation. About 1×104 hEnSCs were cultured in a 35-mm culture dish. Osteogenic differentiation medium included: DMEM/F12, 10% FBS, 1% pen-strep, 7 M dexamethasone, 10 mM β-glycerophosphate, 50 µg/mL L-ascorbic acid-2-phosphate (all materials: Sigma-Aldrich, USA).
14
Two culture dishes were considered as controls and DMEM/F12, 10% FBS, and 1% pen/strep were added to the cells. P3-5 cells were used for injection.
Oil Red O staining
Oil Red O staining was used to confirm the adipogenic differentiation in hEnSCs. First, the cells were fixed with 2% paraformaldehyde and 0.2% glutaraldehyde (15 minutes). After washing with PBS, Oil Red O (#1320-06-5, Sigma-Aldrich, USA) in isopropanol (#67-63-0, Sigma-Aldrich, USA) was added to cells for 10 minutes. The extra stain was removed with 60% isopropanol and then PBS.
14
The presence of lipid droplets, which indicate adipogenic differentiation, was observed under a light microscopy (Zeiss, Germany).
Alizarin red staining
Osteogenic differentiation results in mineralization of the cells. To confirm the osteogenic differentiation, we used Alizarin red staining. The cells were washed by PBS, fixed with paraformaldehyde/glutaraldehyde or 70% ethanol for 15 minutes and then washed with PBS. Alizarin red stain (#TMS-008-C, Sigma-Aldrich, USA) was added to the cells. After washing with 60% isopropanol and PBS, the cells were observed under a light microscopy (Zeiss, Germany).
14
Tracking of injected cells
To confirm the hEnSC homing in the renal tissue and track the injected cells, we labeled hEnSCs with the CM-DiI (#1745878, Life technologies, USA). CM-DiI is a fluorescent marker with high stability and low toxicity. Prior to injection, hEnSCs were washed by PBS and incubated at 5 µM CM-DiI (15 minutes, 37°C and then 20 minutes, 4°C).
15
The cells were centrifuged (5 minutes, 1500 rpm) and then rinsed with PBS. The labeled cells were injected into a separate group of rats (n=6) with AKI. On days 4 and 14, the animals were dissected and kidney and liver were harvested for cell tracking.
Induction of AKI in male Wistar rats
AKI was induced by a single dose of cisplatin (5 mg/kg, IP) in male Wistar rats (n = 18). The animals were kept under standard conditions (22.0 ± 2.0°C, light/dark photocycle) in fiberglass cages with free access to water and food. The rats were divided into the following three groups: sham (n = 6); model (n = 6) that received cisplatin 5 mg/kg of body weight (Mylan, France) via IP to induce AKI; treatment (n = 6) that received approximately 1×106hEnSCs/rat via caudal vein 3 hours after cisplatin injection. Cells were suspended in 200 µL of PBS. Five days after the hEnSC transplantation, all animals were anesthetized by 80-100 mg/kg ketamine, 5-10 mg/kg xylazine (IP), and then sacrificed. Blood sampling and kidney collection were done for subsequent assays.
Biochemical parameter assessment
After clotting at room temperature, blood samples were centrifuged (3000 rpm, 10 minutes) and serums were collected. Serum parameters (i.e. urea, serum creatinine (SCr), and cystatin c (Cst3)) were measured to assess renal function. To evaluate urea, SCr and Cst3 levels, we used urea assay kit (#877-782-3888, BioSystems, Spain), rat creatinine assay kit (#80340, Crystal Chem, USA), and rat cystatin c ELISA kit (#ab201281, abcam, USA), respectively.
Histopathological assay
The kidneys were fixed in 10% formalin solution (#104003, Merck, Germany). Tissue processing was done and tissue samples were embedded in paraffin (#8042-47-5, Merck, Germany) to facilitate cutting. Sections (5-µm thickness) were obtained using a rotary microtome. After staining using hematoxylin and eosin (#105174 and #109844, both Merck, Germany), pathologic tubular damages (including apoptosis, necrosis, debris in the lumen) were scored in 100 tubules for each kidney by a blinded researcher. Zero was given to normal or undamaged tubules, 1 to ˂33% tubular cell injury, 2 to 33%-67% tubular cell injury, and 3 to >67% tubular cell injury.
16
Finally, total pathologic score was obtained by adding all 100 scores and the maximum score was 300.
Immunohistochemical assay for Ki-67 detection
Ki-67 is known as a proliferation marker and is a useful tool for measuring renal tubular cell proliferation.
17
Briefly, 5-µm thickness sections were deparaffinized and rehydrated using xylene (#1330-20-7, Merck, Germany) and ethyl alcohol series. For unmasking of antigens or antigen retrieval, we incubated sections with proteinase K solution (10 minutes, 37°C). Then 3% H2O2 was used for 30 minutes to block or bleach endogenous peroxidases. The mentioned antigen is a nuclear antigen, so the membrane was permeated by Triton x100 (0.5%) for 15-20 minutes. Samples were incubated in bovine serum albumin (BSA) diluted in PBS (2 hours, room temperature). Anti-Ki-67 antibody (#BRB040, Zytomed systems GmbH, Germany) was added to the sections (2 hours, 37°C or overnight, 4°C). Samples were washed by 0.05% Tween 20 + PBS twice after each step. Antibody enhancer was added to the sections for 15 minutes and then the polymer HRP was added for 30 minutes. After washing, the sections were incubated with fresh DAB solution (#DAB500, Merck, Germany) for 3-5 minutes and then nuclei were stained using hematoxylin. Finally, after dehydration and clearing, slides were mounted. Ki-67 positive cells were counted in five images of five non-overlapping fields in each rat by a blinded researcher. ImageJ software (LOCI, University of Wisconsin) was used for data analysis.
Immunofluorescence analysis for CD3+T cell detection
After deparaffinization and hydration of paraffin sections, antigen retrieval was performed using thermal method and Tris Buffered Saline (1X) (2-3 minutes, 2 times). Samples were washed in 0.05% Tween 20 + PBS twice. BSA (5%) was used to block the common antigens of the two species (overnight, 4°C). Anti-CD3 antibody (#sc-20047, Santa Cruz Biotechnology, USA) was diluted in PBS (1:200) and the sections were incubated with the primary antibody at room temperature for 60 minutes. After washing, the slides were incubated with secondary antibody (#ab150077, Abcam, USA) diluted in PBS (1:200) in a dark place at room temperature for 60 minutes. Samples were washed after each step in 0.05% PBS-T. DAPI was used as nuclear counterstain. Finally, the slides were washed 3 times by PBS-T and mounted. CD3 positive cells were counted as described for Ki-67 positive cells.
Real-time PCR
Total RNA extraction from kidney tissue and cDNA synthesis were performed using the extraction kit and the First Strand cDNA synthesis kit (both Maxcell, Iran), respectively. For cDNA synthesis, the RNA mixture (14 µL) and the reaction master mix (6 µL) were mixed and placed in the thermal cycler. Real-time PCR was repeated 3 times. Reaction mixture for real-time PCR included Real Q Plus 2X Master Mix Green (#A324402, Ampliqon, Denmark), primer mixture, and cDNA under the following thermal cycling: 5 minutes at 50°C, 5 minutes at 95°C, and 40 cycles of denaturation for 30 seconds, and annealing/extension at 60-62°C. Relative expression of Il-10 and Cst3 mRNA were calculated using the 2-ΔΔCT method. Gapdhwas considered as internal control. The characteristics of the designed primers are shown in Table 1.
Table 1.
The characteristics of the designed primers for real-time PCR by AlleleID 7.7 software
|
Gene symbol
|
Gene name
|
Sequences 5'→ 3'
|
T
m
|
GC%
|
|
Il-10
| Interleukin 10 |
F: CTGCTCTTACTGGCTGGAGT
18
| 59.35 | 55.00 |
| R: TGGGAAGTGGGTGCAGTTAT | 57.30 | 50.00 |
|
Cst3
| Cystatin c | F: TTTGGATGTGGAGATGGGC | 57.40 | 52.63 |
| R: AGCTGGATTTTGTCAGGGTG | 58.00 | 50.00 |
|
Gapdh
| Glyceraldehyde 3-phosphate dehydrogenase | F: CAAGTTCAACGGCACAGTCA | 57.30 | 50.00 |
| R: CCCCATTTGATGTTAGCGGG | 59.35 | 55.00 |
Tm: Primer Melting Temperature; GC%: The number of G's and C's in the primer as a percentage of the total bases.
Statistical analysis
We used One-way analysis of variance (ANOVA) with Tukey test in GraphPad Prism 8.0.2 software (GraphPad Software Inc., USA) for statistical analysis. Data are presented as mean ± SD. Expression level of mRNA was analyzed using the comparative Ct method. P < 0.05 values were considered statistically significant.
Results
Culture and differentiation of hEnSCs
HEnSCs were plastic adherent, relatively elongated, spindle-shaped cells (). These cells were able to differentiate to osteoblasts and adipocytes ( and ). We used differentiation media for these purposes. According to these findings and flow cytometry results (data not shown), it can be stated that cell extraction was correct. HEnSCs had similar properties to MSCs.
Fig. 1.
Alizarin red and Oil Red O staining of differentiated hEnSCs. (A) Control, (B) osteogenic differentiation, and (C) adipogenic differentiation. HEnSCs were relatively elongated, spindle-shaped cells. These cells were able to differentiate to osteoblasts and adipocytes (scale bar is 100 µm).
Tracking of injected hEnSCs to kidney and liver
In order to ensure the transplantation of hEnSCs to the damaged tissue, and their qualitative tracking, the cells were labeled with fluorescent DiI dye before injection. Tracking of cells in kidney and liver was performed on days 4 and 14 after injection. On day 4, hEnSCs were found mainly in the renal tubules in the cortex and medulla. On day 14 after injection, the number of hEnSCs observed in the tubules increased ().
Fig. 2.
Tracking of transplanted hEnSCs in renal tubules on days 4 and 14. HEnSCs were found mainly in the renal tubules in cortex and medulla. DiI (red) and DAPI (blue) were used for hEnSC labeling and counterstaining, respectively (scale bar: 100 µm).
Tracking of hEnSCs in the left and right lobes of liver tissue on day 4 indicated that a number of injected cells were trapped in the liver. The number of trapped hEnSCs in the liver lobes increased on day 14, which were similar to the results of cell tracking in the kidney ().
Fig. 3.
Tracking of transplanted hEnSCs in liver (top row: right lobe, bottom row: left lobe) on days 4 and 14. A number of injected cells were trapped in the liver. DiI (red) and DAPI (blue) were used for hEnSC labeling and counterstaining, respectively (scale bar: 50 µm).
Changes of serum parameters
On day 5, cisplatin injection increased urea, SCr, and cystatin c, indicating AKI induction. The highest levels of mentioned markers were observed in the model group (248.60 ± 15.06 mg/dL, 1.39 ± 0.17 mg/dL, and 37.26 ± 3.35 ng/mL, respectively), while the baseline levels for these markers in the sham group were significantly lower (52.00 ± 6.18 mg/dL, 0.65 ± 0.09 mg/dL, and 9.50 ± 1.45 ng/mL, respectively). HEnSC injection markedly reduced the levels of renal function parameters (125.40 ± 17.17 mg/dL, 0.86 ± 0.05 mg/dL, and 20.69 ± 2.89 ng/mL, respectively) (Table 2).
Table 2.
Comparison of changes in serum parameters in sham, model, and treatment groups
|
Groups
|
Urea (mg/dL)
|
SCr (mg/dL)
|
Cystatin c (ng/mL)
|
| Sham |
52.00 ± 6.18a
|
0.65 ± 0.09a
|
9.50 ± 1.45a
|
| Model |
248.60 ± 15.06b
|
1.39 ± 0.17b
|
37.26 ± 3.35b
|
| Treatment |
125.40 ± 17.17c
|
0.86 ± 0.05c
|
20.69 ± 2.89c
|
The values are presented as mean ± SD. The letters a, b, and c show a significant difference between the groups (P ˂ 0.05).
Improvement of histopathologic damages after hEnSC injection
Necrosis, apoptosis, debris in the lumen, and hyaline cast formation were assessed as histopathologic lesions in renal tissue. In the model group, cisplatin injection led to a significant increase in pathologic score (154.00 ± 14.95) compared to the sham (105.00 ± 4.56) and treatment (119.40 ± 5.43) groups. The injection of hEnSC reduced the pathological score in the treatment group so that there was no significant difference with the sham group ().
Fig. 4.
Histopathological assay of kidney tissue. (A) Hematoxylin and eosin staining of kidney. HEnSC transplantation led to the repair of histological injuries caused by cisplatin on day 5 (scale bar: 100 µm). (B) tubular injuries include: cell debris in the lumen (black arrow), apoptosis (white circle), necrosis (white triangle), and hyaline cast (white arrow) (scale bars: 50 µm). (C, D) Histograms of pathologic scores and hyaline cast/ HPF, respectively. HEnSC transplantation reduced pathologic scores and hyaline cast formation in treatment group. (a, b) show significant differences between groups (P ˂ 0.05). The values are presented as mean ± SD.
The formation of hyaline cast was another criterion of cisplatin injury in the renal tubules. We did not observe hyaline cast in the sham group, but hyaline cats per high power field (HPF) was 8.00 ± 1.41 in the model group. HEnSC transplantation significantly reduced hyaline casts per HPF in the treatment group (2.50 ± 1.05) ().
Increase of Ki-67 expression in renal tissue after hEnSC injection
One of the criteria for evaluating the effect of injected cells in improving AKI is the rate of cell proliferation in kidney tissue. The cell proliferation marker in tissue, Ki-67, was visible as a brown spot after immunohistochemical staining. In renal tubules, the percentage of Ki-67 positive cells in sham (45.94 ± 3.67) and treatment (39.07 ± 2.95) groups was significantly different from that of the model group (16.61 ± 3.25) (P < 0.05). In glomeruli, hEnSC injection also increased cell proliferation in the treatment group (38.91 ± 5.33), and the expression percentage of Ki-67 was significantly different from that of the model group (23.91± 3.57) ().
Fig. 5.
Proliferation assay in kidney tissue. (A) Immunohistochemical staining of Ki-67 (brown spots), a proliferation marker, in the sham, model, and treatment groups on day 5. HEnSC transplantation increased Ki-67 expression in renal tubules and glomeruli (scale bar: 100 µm). (B, C) Histograms of percentage of Ki-67 positive cells in renal tubules and glomeruli, respectively. HEnSC transplantation increased Ki-67 positive cells in renal tubules and glomeruli in the treatment group. (a, b) show significant differences between groups (P ˂ 0.05). The values are presented as mean ± SD.
Alteration of percentage of CD3+T cells in renal tissue
The percentage of CD3+T cells in renal tissue was assessed using immunofluorescence staining. The CD3+T infiltration after cisplatin injection was significantly increased and the percentage of CD3+T cells was 39.53 ± 3.14% in the model group. CD3+T infiltration after hEnSC transplantation in the treatment group was significantly decreased (28.89 ± 3.66%) compared to the model group. The percentage of CD3+T cells in the sham group was 11.07 ± 2.64 ().
Fig. 6.
Immunofluorescence assay of CD3+T cell infiltration. (A) Immunofluorescence staining of CD3+T cells (green) in kidney in the sham, model, and treatment groups on day 5 (scale bar: 50 µm). (B) Histogram of percentage of infiltrated CD3+T cell. HEnSC transplantation decreased the percentage of infiltrated CD3+T cells in renal tissue in the treatment group. (a-c) show significant differences between groups (P ˂ 0.05). The values are presented as mean ± SD.
Effect of hEnSCs transplantation on mRNA expression of Il-10 and Cst3
The expression levels of Il-10 and Cst3 and their changes after treatment were assessed using real-time PCR (). The upregulation of Il-10 was occurred in the model and treatment groups (1.85 ± 0.07 and 2.57 ± 0.04, respectively) compared to the sham group (1.00 ± 0.40). On day 5 after cisplatin injection, Cst3 was upregulated in the model group (4.76 ± 0.32) compared to the sham group (1.00 ± 0.21). However, upregulation of Cst3 expression was also observed in the treatment group (4.01 ± 0.30), which was less than the model group.
Fig. 7.
Real-time PCR assay of Il-10 and Cst3 expression. (A, B) Histograms of Il-10 and Cst3 expression in the sham, model, and treatment groups on day 5, respectively. Cisplatin injection and cell transplantation caused mRNA expression changes. Transplantation of hEnSCs resulted in the upregulation of Il-10 and downregulation of Cst3 in the treatment group compared to the sham and model groups. The values are presented as mean ± SD.
Discussion
AKI is associated with a variety of problems, including significant morbidity and mortality, the risk of CKD and ESRD, high costs, and reduced survival even in mild injuries. Delays in diagnosis and insufficient treatment lead to increased problems.
19,20
The clinical diagnosis of AKI is usually based on elevated levels of urea/BUN and serum creatinine. SCr depends on age, muscle mass and metabolism, gender, hydration status, and diet. Septic AKI reduces serum creatinine production in muscles. Therefore, SCr may not be a reliable parameter for diagnosing kidney damage.
21
Serum cystatin c, a cystatin protease inhibitor, is filtrated into glomeruli and reabsorbed by proximal tubules. This parameter is a better indicator for diagnosing AKI, because of lower dependence on the mentioned factors and higher sensitivity. Under abnormal conditions, cystatin c levels are inversely related to glomerular filtration rate.
22
In our study, expression of Cst3 gene was significantly increased in the model group and was about 5 times that of the sham group. Cisplatin increased the levels of urea, SCr and cystatin c, which meant AKI induction. Treatment with hEnSCs reduced biochemical parameters of renal function. Thus, serum markers such as urea, creatinine, and cystatin c can be used to diagnose or improve AKI caused by cisplatin.
No specific treatment is available for cisplatin-induced AKI. Even with saline injections before and during chemotherapy, the risk of developing AKI will be 30%.
23
Other platinum-containing chemotherapeutic agents (oxaliplatin or carboplatin) are less nephrotoxic but less effective.
24
Amifostine can reduce the nephrotoxic effect of cisplatin in ovarian cancer, while treatment with amifostine cannot prevent severe nephrotoxicity in most cancers treated with a repeated-low dose of cisplatin.
25
Thus researchers are looking for new treatments. One of the most important therapies that is focused on is the use of stem cells. HEnSCs are new sources for regenerative medicine and cell therapy due to their high proliferative capacity, anti-inflammation secretions, repair ability, specific immunological properties, and differentiation into mesodermal and ectodermal lineages.
14
Given that cisplatin causes nephrotoxicity through inflammation, oxidative stress, tubular and vascular damage, we decided to investigate the role of hEnSCs in reducing inflammation and tubular repair in cisplatin-induced AKI.
Inflammation is an evolutionary and essential response to the elimination of pathogens and the progression of repair after injury, but the resistant inflammation can be harmful. In renal injury, macrophages are absorbed into the affected area. Macrophages secrete large amounts of proinflammatory cytokines and activate other inflammatory cells.
26
In cisplatin-induced renal injury, the release of cytokines by damaged tubular cells and leukocytes lead to initiation and persistence of inflammation. Inflammation is a key factor in cisplatin-induced AKI.
27,28
IL-10 is known as a pleiotropic cytokine with anti-inflammatory and immunoregulatory effects. IL-10 inhibits inflammation and tissue injury by suppressing migration, accumulation, and activation of monocytes and neutrophils. Deng and coworkers showed that IL-10 significantly inhibits cytotoxicity, inflammation, and apoptosis in renal injury. According to their findings, IL-10 reduces cell proliferation and does not appear to restore the renal damage caused by cisplatin. On the other hand, IL-10 may prevent the destruction of renal architecture, and thereby promote cellular function recovery by maintaining cellular scaffold.
29
Wan et al showed that knockout of the IL-10 gene in mice results in increased kidney damage, functional and structural changes in the kidney, decreased proliferation, upregulation of TNF-α and IL-6, and delayed renal repair following IRI. IL-10 can be an important factor in repairing IRI by reducing the production of proinflammatory cytokines.
30
Cisplatin affects the production and/or signaling of IL-10. Cisplatin induces renal inflammation and dysfunction, and the absence of endogenous IL-10 exacerbates these effects. Although cisplatin-induced inflammation increases IL-10 expression in renal resident-dendritic cells, but these cells are a very small percentage of renal cells (less than 0.1%) and IL-10 production by renal dendritic cells alone is not sufficient to protect the kidney.
31
According to our results, Il-10 expression was increased after cisplatin injection, and hEnSC transplantation further increased Il-10 expression. This increase may be due to the anti-inflammatory effects of the hEnSCs themselves or their paracrine effects on the other cells (immune cells and tubular epithelial cells).
The production of anti-inflammatory cytokines such as IL-10 may eliminate post-IRI inflammation and subsequently improve renal repair.
30
In injured mammalian kidney, regeneration or recovery occurs through tubular cell proliferation. It has been shown that transplantation of MSCs can accelerates renal recovery, possibly through paracrine effects.
32
Migration of MSCs to damaged sites and local release of anti-inflammatory, immunomodulatory, and pro-survival factors result in functional and structural improvement, cell proliferation, and reduction of apoptosis.
32,33
According to the findings of Perico et al, hUC-MSCs injection to AKI model caused by cisplatin leads to mitochondrial biogenesis regulation, ATP production, and reinforcement of antioxidant defenses. Due to the high activity of proximal tubular cells in reabsorption, there are many mitochondria in these cells. Metabolic reprogramming of injured proximal tubular cells accelerates tubular cell proliferation and renal repair.
34
HEnSCs tracking revealed that the cells migrated to the damaged sites in the kidney and liver. Evaluation of histopathologic scores, hyaline cast formation, and tubular and glomerular proliferation showed that hEnSCs were involved in renal repair and cell proliferation after cisplatin injection.
Cisplatin increases the infiltration of CD3+T cells and macrophages into renal tissue. Similarly, ischemic/reperfusion injury of kidney induces an early increase in CD3+T cells.
11,12
Dexmedetomidine (alpha2 adrenergic agonist) is able to reduce the immune cell infiltration into renal tissue in response to cisplatin injection. Dexmedetomidine protects the kidney against I/R injury and cisplatin-induced AKI through inhibiting inflammation and apoptosis.
11,35
In line with these findings, we observed an increase in the number of CD3+T cells after cisplatin injection, while the infiltration of CD3+T cells into the kidney was reduced by hEnSCs. In the inflammatory environment caused by cisplatin, proinflammatory cytokines were released from CD3+T cells. HEnSCs reduced infiltration of CD3+T cells into kidney via reducing inflammation.
Conclusion
Cisplatin led to inflammation, uptake of CD3+T cells into the kidneys, histopathologic damage, decreased proliferation of tubular and glomerular cells, and impaired renal function. Following transplantation and migration of hEnSCs, inflammation in the injured kidneys improved, due to the decreased infiltration of CD3+T cells and increased Il-10 expression. Along with these changes, other side effects of cisplatin improved and kidney repair occurred. HEnSCs may ameliorate cisplatin-induced AKI through homing and differentiation, anti-inflammatory and immunomodulatory effects, and/or through paracrine effects, however further research is needed to understand the details of the pathways involved.
Research Highlights
What is the current knowledge?
√ Inflammation is one of the main mechanisms of cisplatin-induced injury in the kidney.
√ Reducing inflammation may improve cisplatin-caused injury in the kidney
What is new here?
√ HEnSCs may ameliorate injuries and repair kidney tissue by immunomodulation and reducing inflammation in cisplatin-induced AKI.
Funding sources
The authors received no financial support for the research.
Ethical statement
This study was approved by the ethical committee of Tabriz University of Medical Sciences (NO. IR.TBZMED.VCR.REC.1397.049).
Competing interests
None.
Authors’ contribution
HZ performed experimental work, data collection and evaluation, data and statistical analysis, and drafting the manuscript. MA performed overall supervision and financial support. PK contributed substantially to the conceptualization and design of the study. RM provided final approval of the version for publication. SEB performed cell isolation and supervision on cellular analyses. MMK collaborated in experimental work.
References
- Transplanted adipose derived mesenchymal stem cells attenuate the acute renal injury induced by cisplatin in rats. Egypt J Histol 2017; 40:169-183. doi: 10.21608/EJH.2017.4075 [Crossref]
- Inhibition of CXCL1-CXCR2 axis ameliorates cisplatin-induced acute kidney injury by mediating inflammatory response. Biomed Pharmacother 2020; 122:109693. doi: 10.1016/j.biopha.2019.109693 [Crossref]
- Acute kidney injury. Annu Rev Med 2016; 67:293-307. doi: 10.1146/annurev-med-050214-013407 [Crossref]
- Dialysis: a review of the mechanisms underlying complications in the management of chronic renal failure. Cureus 2017; 9:e1603. doi: 10.7759/cureus.1603 [Crossref]
- What are the key challenges we face in kidney transplantation today?. Transplant Res 2013; 2(Suppl 1):S1. doi: 10.1186/2047-1440-2-S1-S1 [Crossref]
- Stem cells therapy in general medicine. Electron J Gen Med 2018; 15:em01. doi: 10.29333/ejgm/83014 [Crossref]
- Application of process quality engineering techniques to improve the understanding of the in vitro processing of stem cells for therapeutic use. J Biotechnol 2008; 136:148-55. doi: 10.1016/j.jbiotec.2008.06.009 [Crossref]
- Mesenchymal stem cell therapy in acute kidney injury (AKI): review and perspectives. Rev Assoc Med Bras 2020; 66:s45-s54. doi: 10.1590/1806-9282.66.s1.45 [Crossref]
-
Kim J, Hematti P. Chapter 12: Harnessing Regenerative and Immunomodulatory Properties of Mesenchymal Stem Cells in Transplantation Medicine. Regenerative Medicine Applications in Organ Transplantation: Elsevier; 2014. 163-175. 10.1016/B978-0-12-398523-1.00012-4.
- Endometrial stromal cells exhibit a distinct phenotypic and immunomodulatory profile. Stem Cell Res Ther 2020; 11:1-15. doi: 10.1186/s13287-019-1496-2 [Crossref]
- Dexmedetomidine protects against cisplatin-induced acute kidney injury in mice through regulating apoptosis and inflammation. Inflamm Res 2017; 66:399-411. doi: 10.1007/s00011-017-1023-9 [Crossref]
- Phenotypic and functional characterization of kidney-infiltrating lymphocytes in renal ischemia reperfusion injury. J Immunol 2006; 177:3380-7. doi: 10.4049/jimmunol.177.5.3380 [Crossref]
- Human Endometrial Stromal/Stem Cells Protect Against Cisplatin-Induced Acute Kidney Injury By Inhibition OF Apoptosis In Male Wistar Rats. Cell J 2021; 23:568-575. doi: 10.22074/cellj.2021.7322 [Crossref]
- Endometrial mesenchymal stem stromal cells in mature and immature sheep: An in vitro study. Int J Reprod Biomed 2018; 16:83-92.
- Mesenchymal stromal cells improve renovascular function in polycystic kidney disease. Cell Transplant 2015; 24:1687-98. doi: 10.3727/096368914x684619 [Crossref]
- Severely damaged kidneys possess multipotent renoprotective stem cells. Cytotherapy 2010; 12:303-12. doi: 10.3109/14653241003709645 [Crossref]
- B cells limit repair after ischemic acute kidney injury. J Am Soc Nephrol 2010; 21:654-65. doi: 10.1681/ASN.2009020182 [Crossref]
- Characterization of poly (L-glutamic acid)-grafted hyaluronan as a novel candidate medicine and biomedical device for intra-articular injection. J Biomed Mater Res A 2017; 105:3006-3016. doi: 10.1002/jbm.a.36155 [Crossref]
- Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg 2009; 249:851-8. doi: 10.1097/sla.0b013e3181a40a0b [Crossref]
- Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 2018; 14:607-625. doi: 10.1038/s41581-018-0052-0 [Crossref]
- Urinary biochemistry in the diagnosis of acute kidney injury. Dis Markers 2018; 2018:4907024. doi: 10.1155/2018/4907024 [Crossref]
- Serum cystatin C as a marker of renal function in detection of early acute kidney injury. Indian J Nephrol 2013; 23:180-183. doi: 10.4103/0971-4065.111840 [Crossref]
- Pathophysiology of cisplatin-induced acute kidney injury. Biomed Res Int 2014; 2014:967826. doi: 10.1155/2014/967826 [Crossref]
- The status of platinum anticancer drugs in the clinic and in clinical trials. Dalton Trans 2010; 39:8113-27. doi: 10.1039/c0dt00292e [Crossref]
- Severe neurotoxicity, ototoxicity and nephrotoxicity following high-dose cisplatin and amifostine. Pediatr Hematol Oncol 2005; 22:441-5. doi: 10.1080/08880010590964381 [Crossref]
- The chemokine receptors CCR2 and CX3CR1 mediate monocyte/macrophage trafficking in kidney ischemia-reperfusion injury. Kidney Int 2008; 74:1526-1537. doi: 10.1038/ki.2008.500 [Crossref]
- Restoration of E-cadherin by PPBICA protects against cisplatin-induced acute kidney injury by attenuating inflammation and programmed cell death. Lab Invest 2018; 98:911-923. doi: 10.1038/s41374-018-0052-5 [Crossref]
- Recent Advances in Models, Mechanisms, Biomarkers, and Interventions in Cisplatin-Induced Acute Kidney Injury. Int J Mol Sci 2019; 20:3011. doi: 10.3390/ijms20123011 [Crossref]
- Interleukin-10 inhibits ischemic and cisplatin-induced acute renal injury. Kidney Int 2001; 60:2118-28. doi: 10.1046/j.1523-1755.2001.00043.x [Crossref]
- IL-10 deficiency increases renal ischemia-reperfusion injury. Nephron Exp Nephrol 2014; 128:37-45. doi: 10.1159/000366130 [Crossref]
- Endogenous IL-10 attenuates cisplatin nephrotoxicity: role of dendritic cells. J Immunol 2010; 185:4904-4911. doi: 10.4049/jimmunol.1000383 [Crossref]
- Mesenchymal stem cells in kidney repair. Methods Mol Biol 2016; 141:89-107. doi: 10.1007/978-1-4939-3584-0_5 [Crossref]
- Cell therapy for kidney injury: different options and mechanisms-mesenchymal and amniotic fluid stem cells. Nephron Exp Nephrol 2014; 126:59-63. doi: 10.1159/000360667 [Crossref]
- Human mesenchymal stromal cells transplanted into mice stimulate renal tubular cells and enhance mitochondrial function. Nat Commun 2017; 8:983. doi: 10.1038/s41467-017-00937-2 [Crossref]
- Dexmedetomidine provides renoprotection against ischemia-reperfusion injury in mice. Crit Care 2011; 15:R153. doi: 10.1186/cc10283 [Crossref]